18 year old boy with first episode of siezure.
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment .
CHIEF COMPLAINTS:- Involuntary movements of both upper and lower limbs.
HISTORY OF PRESENTING ILLNESS:-
Patient was apparently asymptomatic 1 day ago , then he developed involuntary movements ,in both upper and lower limbs, which was sudden in onset , associated with shivering,and fever.
He complained of nausea and pain after dinner in the epigastrium which was radiating towards right Iliac fossa and was pricking type with no aggravating and releiving factors.
There was also history of Shortness of breath 1 hr after playing.
At 11.30 pm he was studying, then was feeling uneasy after which he developed involuntary movements of both limbs.
No history of post -ictal confusion, uprolling of eyeballs tongue bite, involuntary defecation, micturition.
PAST HISTORY:-
No history of HYPERTENSION,DIABETES MELLITUS ,ASTHMA, EPILEPSY, TUBERCULOSIS.
PRESENT HISTORY:
•Diet :- mixed
•Appetite:-normal
•Sleep:- adequate(8 hrs/ day)
•Bowel and bladder:- regular
•Addictions:- nil
•Allergy:- nil
Family history :- not significant.
GENERAL EXAMINATION:
Patient was conscious,coherent and cooperative,well oriented to time place and person,moderately built and moderately nourished.
•Pallor:- absent
•Icterus:- absent
•Cyanosis:- absent
•Clubbing:- absent
•Lymph nodes:- absent
VITAL SIGNS:
•TEMPERATURE: Afebrile
•BP:140/80 mm Hg
•RR: 22/min
•Spo2:99
•GRBS:130 mg%
SYSTEMIC EXAMINATION:
☆CVS:S1,S2 heard,no murmurs
☆RESPIRATORY SYSTEM:
•trachea central in position
•Normal vesicular breath sounds heard
•BAE ++
☆CNS EXAMINATION:
●CRANIAL NERVES: INTACT
•Power
Rt UL-5/5. Lt UL-5/5
Rt LL-5/5. Lt LL-5/5
•Tone-
Rt UL -N,Lt UL-N
Rt LL-N,Lt LL-N
•Reflexes:. RIGHT LEFT
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee. ++ ++
Ankle. ++ ++
Plantar:. Flexion Flexion
•SENSORY
crude touch N N
Pain N N
Temperature N N
Fine touch N N
Vibration Right Left
Upper limb. 15 sec 15 sec
Lower limb. 11 sec 10sec
Tibia 14 sec 14sec
Toe 15sec 15sec
Finger nose co-ordination : +
ABDOMEN EXAMINATION:
•Inspection :- no scars
•Palpation :- soft,non tender
•Auscultation :- BOWEL SOUNDS
INVESTIGATIONS:-
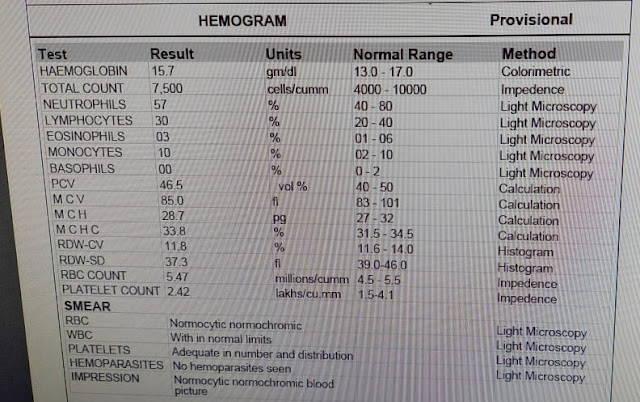
Haemogram:-
Complete Urine Examination:-
Serum electrolytes:-
BLOOD UREA:
Patient's Value:- 23 mg/dl
Normal value:- 12-42 mg/dl










Comments
Post a Comment